Q: What are the most common challenges dentists face in endodontic procedures, and how can these be addressed with the right tools and techniques?
Emily Brennan: Clinically, there are a variety of challenges that dentists face. Let’s first focus on general dentists, especially those who are newer to the profession. A lot of them don't particularly enjoy performing root treatments because of the technical aspects involved. Endodontics tends to have a negative reputation in the industry, often portrayed as a difficult or unpleasant procedure. Oftentimes dentists either love it or hate it.
More experienced general dentists tend to be more confident and are comfortable performing root treatments. However, many of them prefer a single system, and there’s a common misconception about single-file systems; because there’s no such thing as a single-file system that can be used universally for every case. You can’t always predict what file you will need until you open the tooth and examine the canal structure.
Q: How has endodontic technology evolved in recent years, and what impact does this have on the success rate?
EB: Dentists are always aiming for safe, efficient, and predictable results when performing root treatments. In recent years, the use of CBCT scanners has improved both planning and diagnosis. With CBCT, you're no longer working blindly, which is crucial for achieving more predictable outcomes. Even with a microscope, endodontists are still working in the dark to some extent, trying to navigate around curves in the canal, so CBCT has been a game-changer.
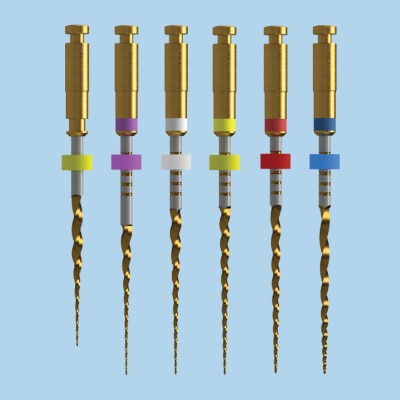
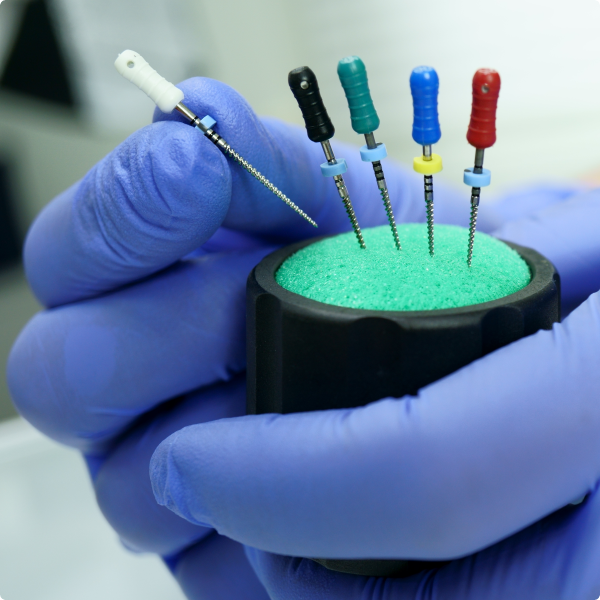
Another significant advancement is in the metallurgy of endodontic files. In the past, hand files were made of stainless steel and used primarily to measure the canal length before introducing rotary files. These mechanical files used to be much stiffer, which made them more likely to break while working in the canal. Today, files are heat-treated, which significantly reduces the chances of file separation or perforation. These improvements in the materials used for files are helping make treatments more reliable and less prone to complications.
There’s also been a huge push in education. There are now more affordable courses available to help general dentists improve their knowledge of endodontics. A big part of this is teaching general dentists to understand their limitations. When I was in practice, we’d often see cases where a file had broken in a tooth, and the patient had to be referred for retreatment. In many cases, I would look at the X-rays and wonder why the general dentist even attempted such a difficult root treatment in the first place. Dentists need to know when it’s time to refer a patient to a specialist.
Even specialists occasionally break files in canals, but specialists are typically able to retrieve broken files much faster than general dentists, which helps prevent delays in treatment.

3D Imaging
A CBCT scanner is a state-of-the-art scanning machine that is used to produce precise, high resolution 3D images of a patient’s mouth including the teeth, jaws, soft tissue and bones – all with high levels of detail.
Q: How can dentists identify and address the causes of endodontic treatment failure?
EB: Endodontic failure is a complex issue, and it's something that endodontists typically need to address clinically, case-by-case. However, there are a few key factors that can contribute to failure and ways to mitigate them. Proper irrigation is essential, as well as the right choice of files and techniques throughout the procedure. The final stages, including obturation (filling the canal with gutta-percha) and sealing, are also critical for a successful outcome. The restoration itself plays a major role in the long-term success of the treatment.
Sometimes, despite the best efforts, things just don’t work. Endodontic failure can be due to a variety of factors, including the difficulty of the case itself. For example, when I was practicing, we’d sometimes tell patients, “You’ve got a 75% chance of success with this treatment.” In those situations, we would often recommend the option of extraction and an implant instead, especially if the root treatment, crown, and post-treatment costs were close to the price of an implant. Sometimes, a 60% success rate on the root treatment just isn't worth it.
Ultimately, diagnosis and case selection are key. Knowing when to proceed with a root treatment and when to consider other options is important for managing patient expectations and ensuring the best possible outcome for patients.
Q: Are there any underutilised products or techniques in endodontics that you wish more dentists knew about?
EB: One thing I would say is the value of a good dental nurse. I cannot stress this enough. When I worked with my boss, we’d spend long hours in the microscope, and it was almost like a silent partnership. We’d have no need to speak — I’d know exactly what he needed, and I’d provide it without question. Over time, he didn’t even need to ask, it was just an unspoken flow.
A huge part of endodontic success comes down to the nurse’s support. In fact, when I was working as an endodontic nurse, 80% of our patients would fall asleep during procedures because we made sure they were comfortable, calm, and reassured. When you have a good, well-trained nurse, the whole procedure becomes so much smoother.